
Health insurers are increasingly limiting coverage for prosthetic limbs, often deeming advanced devices medically unnecessary or experimental, despite their proven benefits. This trend has significant implications for amputees seeking to regain mobility and quality of life.
Coverage Limitations and Denials
Many insurance plans impose caps on durable medical equipment (DME), including prosthetics, with annual limits ranging from $1,000 to $5,000. These caps are often insufficient to cover the full cost of advanced prosthetic devices, which can be significantly higher.
Additionally, insurers may deny coverage by labeling certain prosthetics as not medically necessary or experimental, even when such devices have been in use for years. For instance, microprocessor-controlled knees, which enhance stability and mobility, are sometimes excluded from coverage despite their established efficacy.
Impact on Amputees
These coverage limitations can delay or prevent access to essential prosthetic care. Fewer than half of individuals with limb loss have been prescribed a prosthesis, partly due to insurance denials.
In a recent case, a Utah family sought insurance approval for a $24,000 bionic arm for their 9-year-old daughter, Remi Bateman, who was born without a hand. Their insurer denied the request, deeming the device not medically necessary, highlighting the challenges families face in securing coverage for advanced prosthetics.
Medicare and Medicaid Policies
Medicare covers prosthetic devices when ordered by a Medicare-enrolled doctor, with Part A covering inpatient procedures and Part B covering outpatient procedures. However, beneficiaries are typically responsible for 20% of the Medicare-approved amount, which can still be a substantial out-of-pocket expense.
Medicaid coverage for prosthetics varies by state, with some programs imposing their own limitations and requirements, potentially affecting access to necessary devices.
Advocacy and Legislative Efforts
Advocacy groups, such as the Amputee Coalition, are pushing for insurance fairness for amputees, seeking to eliminate restrictive caps and ensure comprehensive coverage for prosthetic devices. They argue that access to appropriate prosthetic care is essential for individuals to lead independent and productive lives.
Legislative efforts at both state and federal levels aim to address these disparities, striving to mandate more inclusive coverage policies that consider the functional needs and potential of prosthetic users.
Conclusion
The limitations imposed by health insurers on prosthetic limb coverage present significant obstacles for amputees seeking to improve their mobility and quality of life. Ongoing advocacy and policy reforms are crucial to ensure that individuals requiring prosthetic devices receive the support and coverage necessary to access appropriate and effective care.
Family Appeals for Coverage of Daughter's Prosthetic Arm






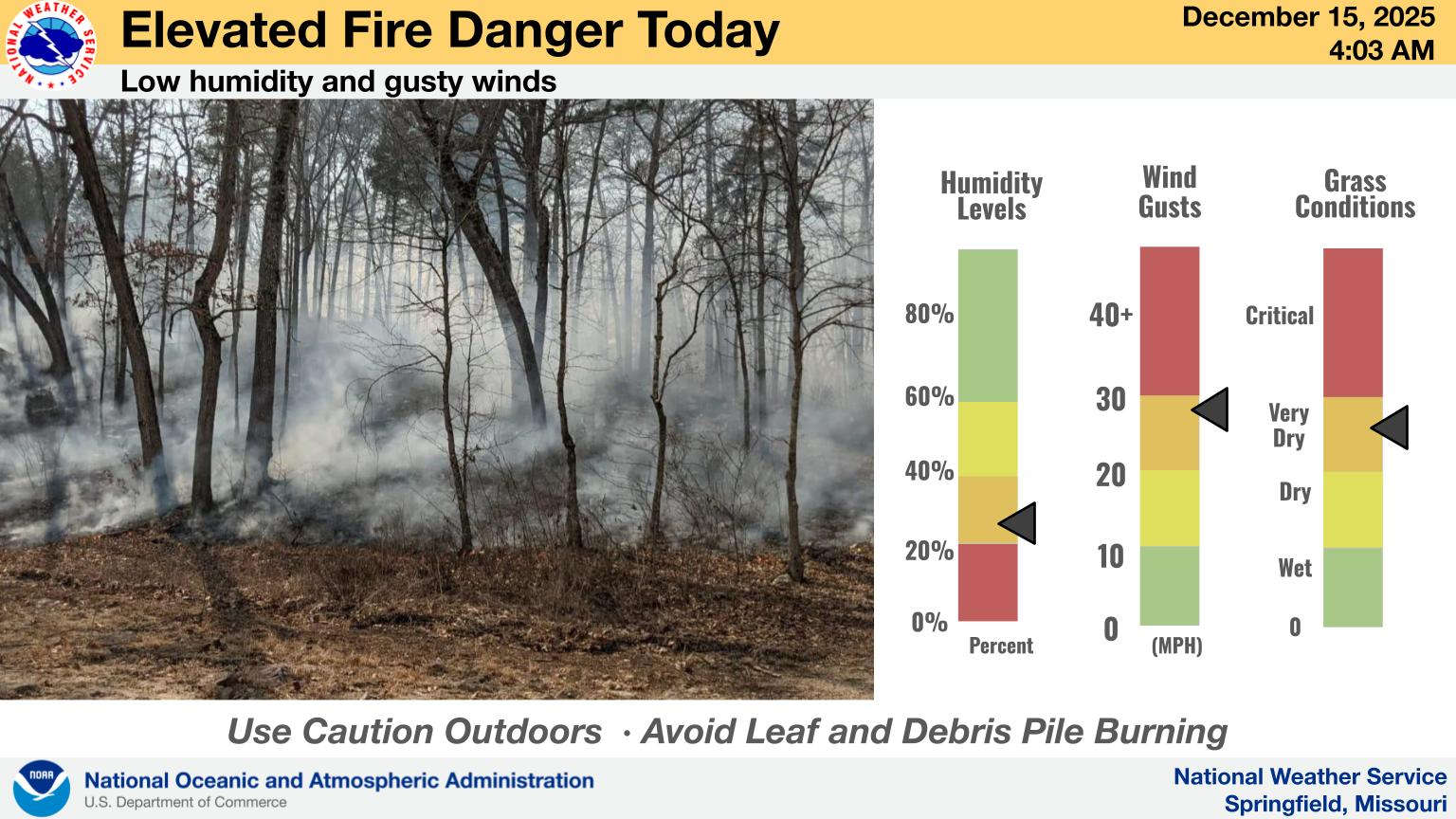 NWS Warns of Fire Danger
NWS Warns of Fire Danger
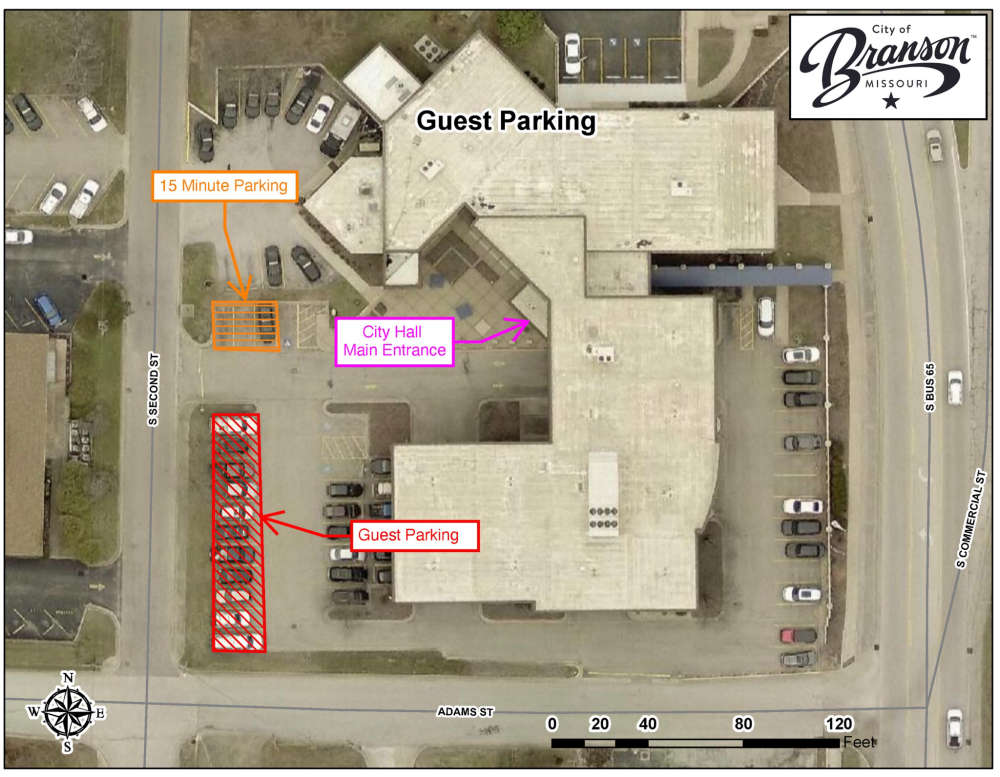 Branson City Hall Update Begins This Week
Branson City Hall Update Begins This Week
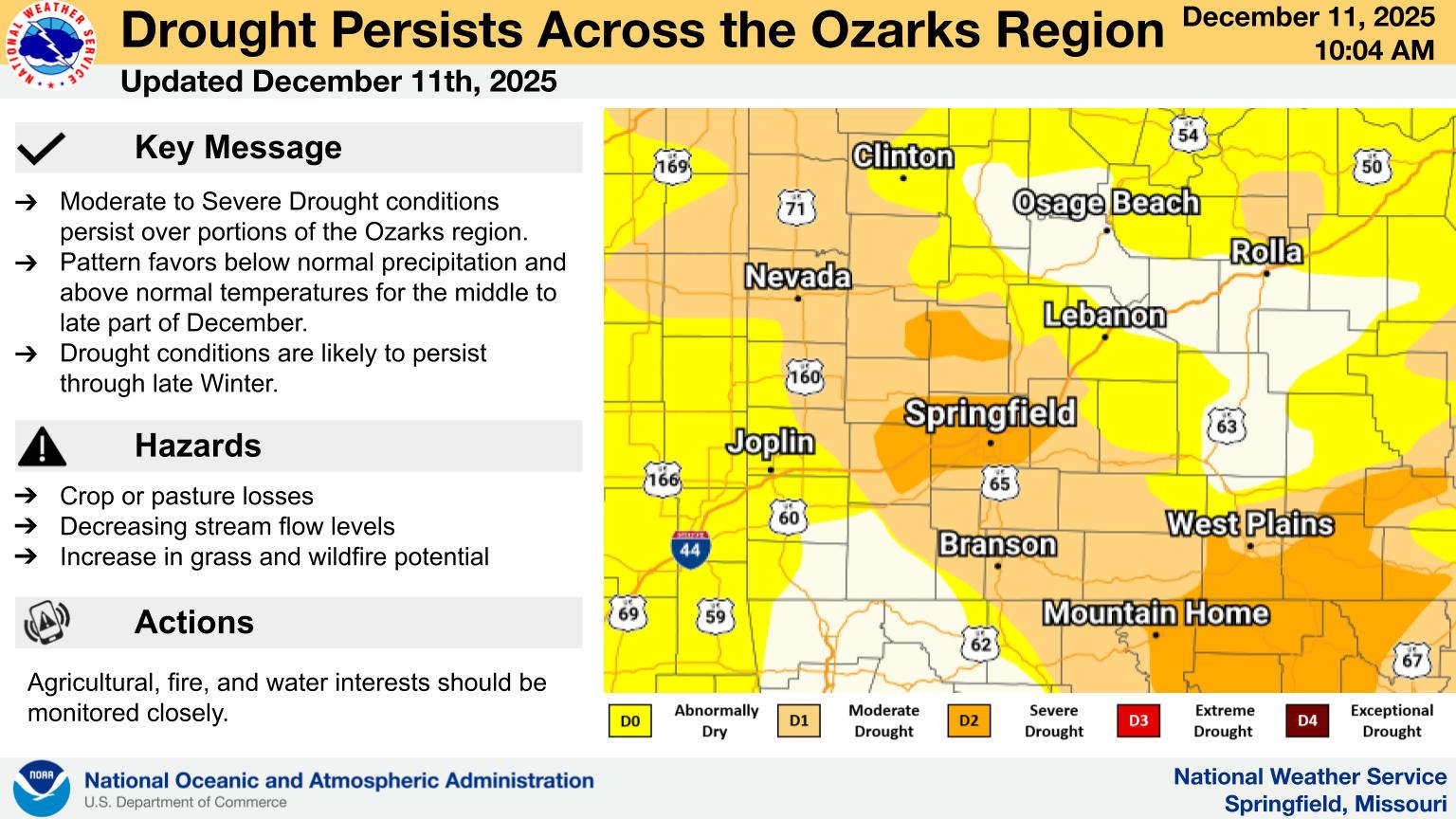 Drought Conditions Remain Steady Across the Lakes Region
Drought Conditions Remain Steady Across the Lakes Region
 Arkansas Public Television to End Affiliation with PBS
Arkansas Public Television to End Affiliation with PBS